“Enhancing Surgical Precision in Head and Neck Cancer with Intraoperative Fluorescence Imaging”

Nitish Khurana, PhD
Research Assistant Professor, Department of Molecular Pharmaceutics, University of Utah
View Bio
▼
Nitish Khurana, Ph.D., is a Research Assistant Professor in the Department of Molecular Pharmaceutics at the University of Utah College of Pharmacy. His research focuses on the development of translational nanomedicine and imaging technologies for cancer prevention, treatment, and critical care. He has broad expertise in drug delivery, biomaterials, and image-guided oncology, with an emphasis on advancing technologies from bench to bedside. One of Dr. Khurana’s current work centers on fluorescence-guided surgery for oropharyngeal squamous cell carcinoma, where he is investigating the use of indocyanine green (ICG) and engineered extracellular vesicles to improve intraoperative tumor margin visualization and enable real-time disease detection. He has authored multiple peer reviewed publications and actively contributes to multidisciplinary collaborations at the interface of pharmaceutics, oncology, and pharmacological sciences. His long-term goal is to establish an independent research program focused on developing innovative imaging and drug delivery platforms that enhance precision cancer care and patient outcomes.
“Advancing Precision Health Symptom Science Through the Evaluation of Biological, Social, and Environmental Risk Factors in Patients Living with Cancer”

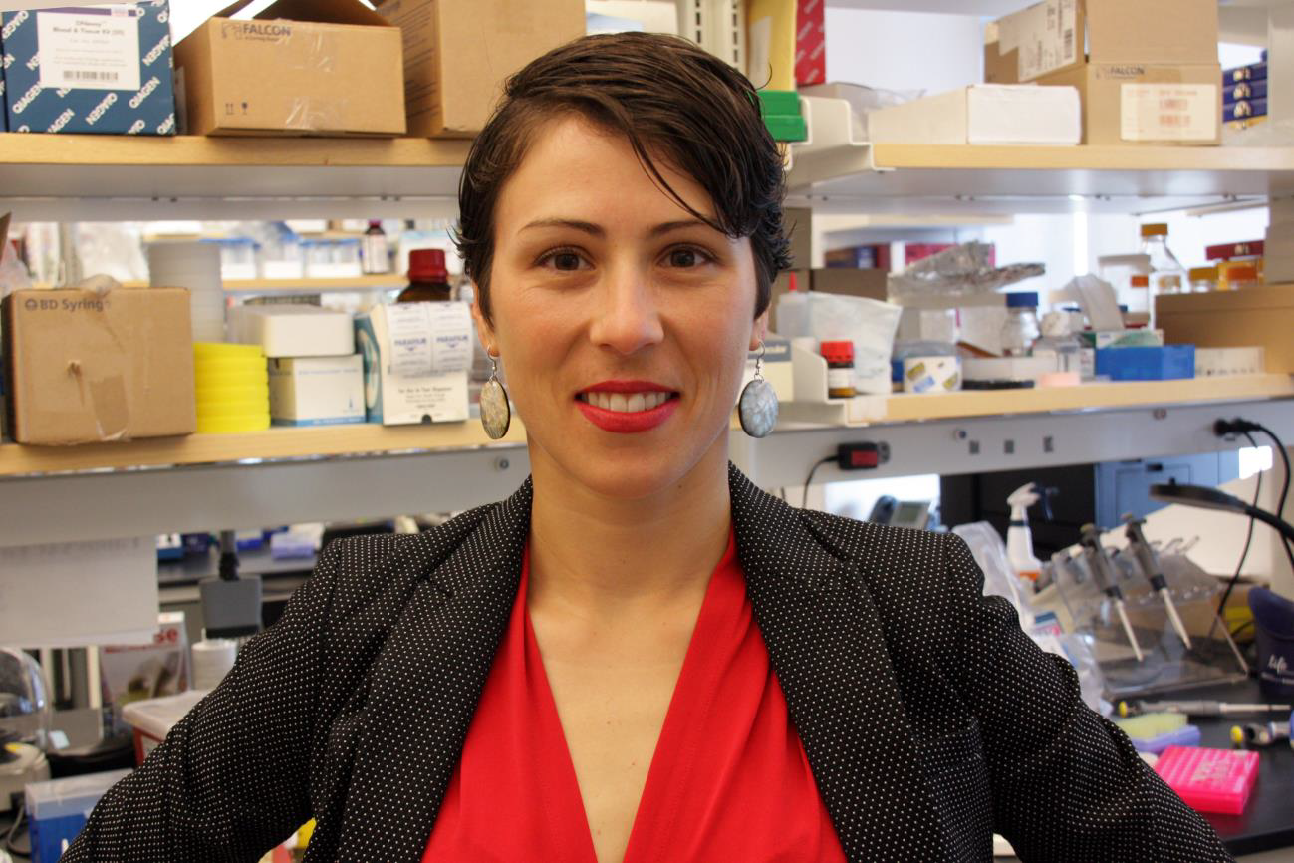
Carolyn Harris, PhD, RN
Assistant Professor, Department of Physiological Nursing, School of Nursing, University of California, San Francisco
View Bio
▼
Dr. Carolyn Harris is an Assistant Professor in the Department of Physiological Nursing at the University of California, San Francisco School of Nursing. Her program of research is focused on evaluations of the biological, social, and environmental factors that underlie single symptoms and symptom clusters in patients living with cancer. This research will lead to the development and testing of personalized interventions for patients undergoing cancer treatment to prevent or ameliorate this symptom burden. Currently, she is leading projects to characterize the symptom experience of patients with cutaneous melanoma receiving immune checkpoint inhibitor therapy and evaluate the influence of attributes within the social and built environment on symptom burden in oncology patients receiving chemotherapy. Dr. Harris received a PhD in Nursing from the University of California, San Francisco and completed two postdoctoral fellowships at the University of Pittsburgh (NCI Pathway to Independence Award for Early-Stage Postdoctoral Researchers, K99CA286967; Targeted Research and Academic Program for Nurses in Genomics, T32NR009759).
Register Now